LASER-LIPO: INVASIVE TECHNOLOGY
Content extracted from the book “Victory Against Cellulite” by Dr Roberto Chacur, Ed. AGE, 2023.
Use of technologies associated with plastic surgery for the treatment of cellulite
Dr. Luciene Oliveira
Dr. Roberto Chacur
INTRODUCTION
Cellulite is a common cosmetic condition that affects most women. It is characterized by the non-homogeneous appearance of the skin covering the glutes and the posterior region of the thigh. Its multifactorial etiology requires multidisciplinary treatment and follow-up. It is known that, in anatomical terms, the irregularities and nodules caused by cellulite require subcutaneous adipose tissue for their base, fat herniation by the weakened fibrous septa of the subcutaneous associated with the looseness of the connective tissues that allow the skin to be pulled and the irregularities perceived (WHIPPLE et al., 2019). Treatments that associate the reduction of adipose tissue and also the sagging of tissues are excellent allies for the resolution of cellulite. Liposuction, one of the most performed surgeries in the world, evolved from an intervention that removed small amounts of localized fat to a surgery capable of modeling and modifying the patient’s body. Associated with technological evolution, such as Bodytite, Mopheus and Renuvion resources for tissue retraction, it has become an important tool in body outline management and in the treatment of irregularities caused by cellulite, such as skin retraction after liposuction with Renuvion.
See Chapters
CHAPTER 1 - DEFINITION, HISTORY AND NOMENCLATURE
CHAPTER 2 - ONLINE QUESTIONNAIRE FOR CELLULITE CLASSIFICATION
CHAPTER 3 - LIPEDEMA: DESCRIPTION, DIAGNOSIS AND TREATMENT
CHAPTER 4 - ANATOMY OF THE GLUTE REGION APPLIED IN PRACTICE
CHAPTER 6 - INJECTABLE CELLULITE TREATMENTS
CHAPTER 7 - LASER-LIPO: INVASIVE TECHNOLOGY
CHAPTER 8 - OTHER CELLULITE TREATMENTS
CHAPTER 9 - BIOSTIMULATORY EFFECTS OF MICROSPHERE INJECTIONS INTO OVERLYING SKIN STRUCTURES
CHAPTER 10 - INFLUENCE OF HORMONES ON CELLULITE: WITH EMPHASIS ON ADIPONECTIN
CHAPTER 11 - GOLDINCISION®: A MULTIFACTORIAL APPROACH TO THE TREATMENT OF CELLULITE
CHAPTER 12 - STAINS POST-GOLDINCISION®
CHAPTER 13 - ADVERSE EFFECTS AND COMPLICATIONS IN GOLDINCISION®
With the collaboration of experienced medical professionals, Dr. Roberto Chacur brings together in this book an approach around the theme ranging from the genesis of cellulite, the proper method of evaluating and classifying, associated diseases and hormonal modulation to existing treatments, what really works and why the GOLDINCISION method is considered the gold standard.
CELLULITE ANATOMY
Anatomical studies (RUDOLPH et al., 2021) have investigated the architectural arrangement of the subcutaneous tissue in the glute and related biomechanical properties. Using full-thickness sections, five different layers over the gluteus maximus (dermis, superficial fat, superficial fascia, deep fat, and deep fascia) and two different types of septa (numerous short, thin septa connecting the superficial fascia to the dermis and less long, thick septa connecting the deep fascia to the dermis and carrying neurovascular bundles). Both the superficial and deep fat layers formed a honeycomb-like structure of fat lobules surrounded by fibrous connective tissue.
The three-dimensionality of a subdermal septum provides important clinical clues for understanding the underlying mechanisms and pathogenesis of cellulite. The 3-D approach, in contrast to previous 2-D models, presents a robust basis for understanding and developing therapeutic strategies for cellulite (SMALLS et al., 2005).
The study revealed an interaction of structural features with biomechanical properties at the subdermal junction (ie, between the dermis and the subcutaneous adipose tissue). This interactive relationship between the support offered by the dermis (collagen), the type and number of septal connections (fibrosis) and the architecture of the fatty layer (amount of fat) determine the presence or absence of cellulite. This delicate balance is further influenced by gender, increasing age and high body mass index, which are all recognized risk factors for cellulite (NÜRNBERGER & MÜLLER, 1978, HEXSEL et al., 2009; PIÉRARD et al., 2000; MIRRRASHED et al., 2004; DOBKE et al., 2002; LESZKO, 2014).
Increasing age resulted in significant thinning of the dermis, regardless of gender, providing less support to contain the underlying fatty layers. These findings aligned line with clinical findings showing that increasing age and skin sagging are related to increased prevalence and/or worsening of cellulite (DOBKE et al., 2002; LESZKO, 2014; DE LA CASA ALMEIDA et al., 2013; ORTONNE et al.).
Higher body mass indexes (BMI) resulted in an increase in the thickness of both superficial and deep fat, increasing the height of the lobe, but not so much its width. These increases can upset the delicate balance between containment and extrusion forces at the subdermal junction that favor extrusion, in addition to the increase in biomechanical instability attributable to fewer septal connections, increased fat lobe height, and thinner skin. Obese and elderly women are highly predisposed to the presence and worsening of cellulite (LUEBBERDING et al., 2015; FRIEDMANN et al., 2017; ROSSI & VERGNANINI, 2000).
IMPORTANT CONSIDERATIONS
• The maximum safe volume for most patients is 300 ml per session; this amount must never be exceeded. We always recommend using volumes smaller than the aforementioned 300 ml per session, especially in case the professional has less experience.
• It is always better to use smaller amounts of product and a larger number of sessions.
• As a rule, the patient does not need to discontinue any of the medications of continuous use.
• Absolute contraindications for glute filling include: pregnancy, any pathology under treatment or not yet treated, according to medical evaluation.
• Relative contraindications are nephropathy, autoimmune disease, coagulopathies, extremely atopic patients, underage patients (only authorized and accompanied by parents and when indicated and absolutely necessary).
• The correction must be made with the minimum amount of product necessary.
• Pay attention to muscle contractures; when observed, the procedure should be suspended, anti-inflammatories and/or muscle relaxants should be prescribed, and the patient should be advised to return in 30 days to complete the filling.
• In the case of a patient with no skin sagging in the gluteal region, a fact observed during the physical examination in the face-to -face evaluation, preferably, the maximum volume of 120 ml of filling should never be exceeded on each side of the glute in each filling session for correction needed.
• When low muscle density is observed, making it impossible to maintain the filling procedure in the superficial muscular plane, to perform the necessary correction, one should not exceed 100 ml of filling volume on each side per session.
• Pay attention to any postural hypotension during the procedure, since the patient remains most of the time in an orthostatic position. Don’t forget that most people have pressure drops when undergoing simple lab tests.
• Check vital signs before carrying out the procedure, such as BP, especially in older patients or those with a history of SAH.
• After the filling procedure, we massage with moderate compression in the places where it was filled, after having placed a small bandage in each of the orifice areas. The bandage must be kept for 24 hours.
• The trochanteric area should always be massaged to minimize the risk of product accumulation, which can generate nodules and granulomas. The patient should be advised about edema after the procedure.
• The buttocks are usually higher (“pouty”) in the immediate post-procedure period, due to muscle contracture, which tends to increase a little more in subsequent days. Inform the patient that this aspect tends to improve in the following two weeks and that the result will be more rounded than in the immediate post-procedure period. Always prescribe the use of prophylactic antibiotics, associated with anti inflammatories, for 3 to 5 days, and a more powerful analgesic (SOS) in case of more severe pain. Muscle relaxants are a great option in case of more marked contracture and in patients with more painful symptoms.
• It is important to remember that opioid analgesics can cause dizziness and muscle relaxants can make the aptient sleepy.
• New approaches can be performed after 30 days, in case of absence of discomfort and absence of muscle contracture on physical examination. It is important to always maintain contact with the patient.
• The patient carries a labeled folder containing the batch/expiry date of the product that was used, along with the post-procedure instructions and the doctor’s contact information.
• The patient should be instructed that the volume in the immediate post-procedure usually decreases and that in most cases there is a need for a new approach to obtain the desired result. In relation to the gluteal filling areas, we highlight some particularities of clinical relevance:
• It is known that the most successful technique for performing a central or peripheral venous or arterial access is the puncture along the path of the blood vessel. We observed that the blood vessels in the gluteal region commonly run in favor of the muscle fibers, that is, parallel to them. Thus, we conclude that the safest way to perform the filling is through perpendicular openings to the area to be corrected, thus making the application safer.
• The superolateral region of the gluteal region is relatively free of nerves and vessels, making it safer.
• The region of the trochanteric area, due to the low amount of fat, is a region in which the product must be very well distributed, in order to avoid the presence of nodules and granulomas.
• The inferomedial region of the glutes is the area of emergence of nerves and vessels, which commonly exit in the deep plane; therefore, when working on this region, one should always work on the superficial muscular plane, with the smallest amount of product necessary, always keeping it well distributed.
COLLAGEN
Collagen is an important body protein, representing between 25 and 30% of all body protein. This fibrous protein is made up of peptide chains formed by amino acids, such as glycine, proline and hydroxyproline. It is known that from the age of 30 this protein progressively decreases in the body, and therefore patients begin to show signs of skin sagging.
Collagen fibrils are formed through the polymerization of tropocollagen (molecular units). Tropocollagen is made up of three polypeptide chains, which are arranged in a triple helix. Tropocollagen aggregates into microfibrils, which join to form fibrils in collagen types I, II, and III. In types I and III, these fibrils form the fibers. Knowledge of the relationship between the various layers of the skin, mainly the dermis and hypodermis, and the changes they undergo during aging is essential for understanding sagging skin, the mechanism of action and indications for treatments for sagging. In chronological aging, the thickness of the dermis decreases as a result of biochemical and structural changes in collagen and elastic fibers, as well as in the fundamental substance (ROSSI & VERGNANINI, 2000; FLORY & GARRETT, 1958).There is a reduction in collagen synthesis and an increase in its degradation, due to the increase in collagenase levels.
The cutaneous collagen content is reduced by about 1% per year throughout adult life, beginning around the age of 40 in women an
a little later in men. The remaining collagen fibers are disorganized, more compact and fragmented. Elastic fibers decrease in number and diameter. The amount of ground substance mucopolysaccharides is reduced, especially hyaluronic acid. These changes negatively influence skin turgor and collagen (MIRRASHED et al., 2004), while the hypodermis presents thinning caused by aging.
Technologies that stimulate collagen formation and body remodeling, improving cellulite irregularities based on thermal modification (shrinking) of connective tissue are widely used in the area of aesthetics.
The latest innovations have enabled even better results. Usually applied through the skin, the forms of application using new technologies require that many tissues be crossed to reach the place to be treated, losing intensity and results along the way. To compensate, technological innovations allowed the emergence of minimally invasive devices that could be directly applied to the site to be treated, providing greater energy, better results and more safety. The physical effects of heat on collagen are well known, an action that must be performed at temperatures necessary to alter collagen molecular binding and thus cause tissue shrinkage (65 to 70°C). It is also known to destroy cell viability. Thermally modified tissues are devitalized and must undergo a process of biological remodeling and repair, with a view to reducing redundant tissue and, therefore, reducing flaccidity.
HEAT COLLAGEN STIMULATION
The type I collagen molecule, the main structural component of the dermis, is formed by three polypeptide chains, in a triple helix, which are stabilized by intramolecular cross-links. These molecules are in turn aggregated in a parallel pattern to form collagen and fibrin. This three dimensional arrangement is maintained by intermolecular crosslinks and gives the tissue its tensile properties. Intramolecular crosslinks are reducible covalent aldehyde bonds, which, during the aging process, are progressively replaced by irreducible multivalent crosslinks. When collagen is heated, the thermolabile intramolecular cross-links are broken, and the protein undergoes a transition from a highly organized tissue to a random, gel-like state (denaturation) (Fig. 7.1).
At the macroscopic level, the effect of heat can be summarized as shrinkage along an axis parallel to the dominant direction of fiber orientation, accompanied by dilation in the transverse axis, that is, densification of tissues that are structured by collagen and its contraction, allowing greater rigidity to the tissue. Scientific works have established that when collagenous tissues are exposed to high temperatures (in the range of 65 to 85°C for most tissue types and species), they undergo rapid denaturation (FLORY & GARRETT, 1958). The resulting effect of the microscopic phenomenon of collagen denaturation is tissue shrinkage (ALLAIN et al., 1980). At a constant temperature, shrinkage increases with increasing exposure until it reaches a plateau value beyond which no further shrinkage is observed. Heating at excessive temperatures for long periods of time results in hyalinization, thermal damage and tissue necrosis (LE LOUS et al., 1985).
The healing process and biological repair of tissues treated with heat-based technologies will result in a decrease in volume and area of the treated tissue, hence the effect of skin contraction.
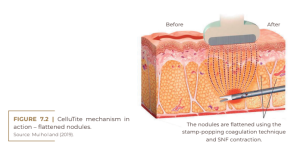
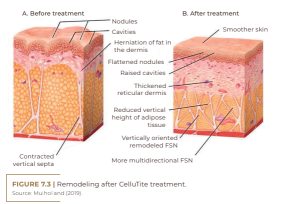
This is invasive radiofrequency using bipolar tips. Radio frequency energy is a form of electromagnetic energy. When applied to tissues, the rapidly oscillating electromagnetic fields cause movement of charged particles within the tissue, and the molecular result of the movement generates heat, and this heat will modify collagen, but it will also allow the destruction of fat cells, improving and regularizing the subcutaneous tissue, and reducing the orange peel appearance of the skin. The BodyTite® device comprises a workstation, or platform, which houses the radiofrequency generator, the software and the circuit boards of the system. Each BodyTite® handpiece is in a bipolar configuration, where the inner electrode is a silicon-coated cannula that emits radiofrequency in its uncoated region distal to the outer electrode (Figure 7.2).

BodyTite and the BodyTite tip (Source: Plast Reconstr Surg Glob Open (2020).
The inner electrode emits positively charged radiofrequency current, which flows towards the negatively charged outer electrode. Radiofrequency is strongly ablative and coagulative within 1-2 cm of the inner electrode, dissipates in its flows and diffuses to the outer electrode. The soft tissue within 1-2 cm of the inner electrode will undergo a necrotic and tissue ablative thermal effect, while the dermis will experience a subnecrotic non-ablative thermal stimulation. Radiofrequency energy within 1-2 cm of the inner electrode provides a coagulative and ablative emission in local tissue, adipose, vascular and in the fibroseptal network, which will generate subsequent regeneration and contraction of these tissues. The procedure can be performed in the operating room or in the practice.
MORPHEUS 8: MICRONEEDLE RADIOFREQUENCY
The Morpheus 8 is designed to deliver RF energy to the skin in a non-homogeneous fractional manner via a 40-electrode pin array on the body. The matrix delivers bipolar radiofrequency energy to the skin, resulting in its heating around the contact of the electrodes, to temperatures that lead to electrocoagulation and homeostasis of small portions of the skin. The procedure is performed leaving untouched areas between the pin electrodes, which maintain the integrity of the treated skin and serve as a reservoir of cells that promote and accelerate the healing process. The system provides individual adjustment of treatment parameters to achieve maximum efficiency and safety for each patient and need, generating three-dimensional tissue remodeling (skin contraction by area and volume contraction by fat reduction). It can be performed in a surgical block or in the medical practice, with topical anesthesia. According to Robert Stephen Mulholland (MULHOLLAND, 2019), Morpheus 8 “uses the proven soft tissue contraction of BodyTite in a non- invasive external procedure”. According to the specialist, “it inserts up to 40 positively charged coated electrodes of 8 mm in the subcutaneous soft tissue. A monopolar ablative lesion is generated from the tip of the electrode, stimulating NSF contraction and adipose coagulation. The RF then flows to distant negative return electrodes on the surface of the skin, providing non-ablative thermal stimulation to the papillary dermis.”
The burst feature of Morpheus is known to provide multiple simultaneous levels of internal clotting. Mulholland concludes that, according to studies, “the combination of internal BodyTite thermal coagulation and external Morpheus 8 simultaneous to liposuction can result in 60 to 70% contraction of the skin area, greatly improving soft tissue contours and body shaping results after liposuction procedures. The Morpheus group of applicators and soft tissue reshaping tips has quickly become a widely used tool worldwide to achieve fractional skin tightening, as well as wrinkle reduction and soft tissue remodeling. Mulholland compares Morpheus to a handshake between BodyTite, Facetite and Accutite RFAL and Fractora, “considering that Fractora is external, percutaneous DERMAL RFAL, while Morpheus is external RFAL applied to the adipose and subdermal space” (Figure 7.5).
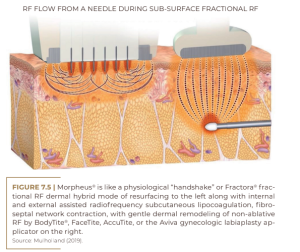
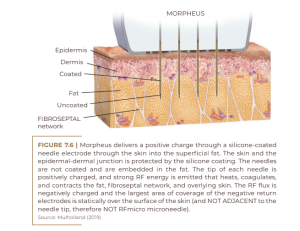
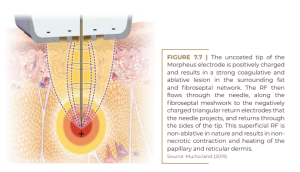
In order for Morpheus to flow and induce soft tissue contraction, the handpiece provides 24 pins (when facial) of silicone-coded RF-emitting electrodes, which act on the surface culture under the skin when a proprietary pulse of energy is released. radiofrequency electrical technique, which coagulates the subdermal adipose tissue and strengthens the horizontal, oblique and vertical connections with the skin, called FSN, providing significant smooth skin tightening and reducing overlying wrinkles, scars, uneven textures, pores and stretch marks. Coated needles play the important role of protecting the skin from any thermal injury (Figures 7.6 and 7.7).
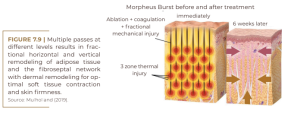
What is the Morpheus Burst? It is an automated multiple fractionated vertical adipose RFAL ablation in a single-cycle coagulation. Penetration of up to 7 mm of ablation and 8 mm of heat allows the use of the Morpheus 8 applicator at multiple levels during the same insertion cycle (Figure 7.8).
Each Morpheus Burst pulse corresponds to three sequential passes, resulting in three times the ablative and coagulative index, as well as a significant increase in soft tissue contraction (Figure 7.9). The Morpheus 8 family of adipose and dermal fractional RFAL ablation has become the most successful and widely used set of fractional ablative devices worldwide.

RENUVION
The Renuvion is a device that looks like a pistol with a cannula, which is introduced under the patient’s skin through an incision similar to that of a liposuction, between 0.5 and 1.0 cm, in the regions where there is a desire to treat sagging.
The device mixes helium gas and radiofrequency, which together generate what we call a plasma jet. By applying this jet of plasma under the skin, Renuvion reduces the fibrous septa that lie beneath the skin, immediately causing the skin to retract, minimizing sagging and herniation of the fatty tissue.

In addition to this immediate effect, there is also a secondary effect, between 6 and 9 months of collagen stimulation in this region, which will also cause skin retraction and improve the final results. This device has the drawback that it can only be used in a surgical block.
CONCLUSION
Surgery and technology are excellent allies in the treatment of cellulite. Liposuction is a safe, controlled and definitive way to reduce the subcutaneous adipose tissue, while the technologies are responsible for the contraction of the fibrous septa and the stimulus for collagen. The results and their maintenance will depend on the intrinsic characteristics – metabolism, hormones, age – and on the care that the patient will have in the postoperative period. Healing is a well-orchestrated natural and biological process, and the end result will depend on this repair. By balancing the magnitude of the surgical insult against the tissue’s ability to repair, we will achieve the best results.
REFERENCES
Allain JC, Le Lous M, Cohen-Solal L, Bazin S, Maroteaux P: Isometric tensions developed during the hydrothermal swelling of rat skin. Connect Tissue Res 1980;7:127-133.
Chvapil M, Jensovsky L: The shrinkage temperature of collagen fibres isolated from the tail tendons of rats of various ages and from different places of the same tendon. Gerontologia 1963;1:18-29.
Chvapil M, Jensovsky L: The shrinkage temperature of collagen fibres isolated from the tail tendons of rats of various ages and from different places of the same tendon. Geron- tologia 1963;1:18-29.
De La Casa Almeida M, Suarez Serrano C, Rebollo Roldán J, Jiménez Rejano JJ. Cellulite’s aetiology: A review. J Eur Acad Dermatology Venereol. 2013;27:273-278. Dobke MK, Dibernardo B, Thompson RC, Usal H. Assessment of biomechanical skin properties: Is cellulitic skin different? Aesthet Surg J. 2002;22:260-266.
Flory PJ, Garrett RR: Phase transitions in collagen and gelatin systems. J Am Chem Soc 1958;80:4836-4845.
Friedmann DP, Vick GL, Mishra V. Cellulite: A review with a focus on subcision. Clin Cosmet Investig Dermatol. 2017;10:17-23. Hexsel DM, Abreu M, Rodrigues TC, Soirefmann M, do Prado DZ, Gamboa MM. Side-by-side comparison of areas with and without cellulite depressions using magnetic resonance imaging. Dermatol Surg. 2009;35:1471-1477.
Le Lous M, Cohen-Solal L, Allain JC, Bonaventure J, Maroteaux P: Age related evolution of stable collagen reticulation in human skin. Connect Tissue Res 1985;13:145-155. Leszko M. Cellulite in menopause. Prz Menopauzalny 2014;13:298–304.
Luebberding S, Krueger N, Sadick NS. Cellulite: An evi- dence-based review. Am J Clin Dermatol. 2015;16:243-256.
Mirrashed F, Sharp JC, Krause V, Morgan J, Tomanek B. Pilot study of dermal and subcutaneous fat structures by
MRI in individuals who differ in gender, BMI, and cellulite grading. Skin Res Technol. 2004;10:161-168. 128 The victory against cellulite
Mulholland, RS. “BodyTite®: The Science and Art of Radiofrequency Assisted Lipocoagulation (RFAL) in Body
Contouring Surgery.” The Art of Body Contouring. In-tech-Open, 2019.
Nürnberger F, Müller G. So-called cellulite: An invented disease. J Dermatol Surg Oncol. 1978;4:221-229. Ortonne JP, Zartarian M, Verschoore M, Queille-Roussel C, Duteil L. Cellulite and skin ageing: Is there any interaction? Piérard GE, Nizet JL, Piérard-Franchimont C. Cellulite: From standing fat herniation to hypodermal stretch marks. Am J Dermatopathol. 2000;22:34-37. Rossi AB, Vergnanini AL. Cellulite: A review. J Eur Acad Dermatol Venereol. 2000;14:251-262. Rudolph C, Hladik C, Hamade H, Frank K, Kaminer MS, Hexsel D, Gotkin RH, Sadick NS, Green JB, Cotofana S. Structural
Gender Dimorphism and the Biomechanics of the Gluteal Subcutaneous Tissue: Implications for the Pathophysiology of Cellulite. Plast Reconstr Surg. 2019 Apr;143(4):1077-1086. doi: 10.1097/PRS.0000000000005407. PMID: 30730492.Smalls LK, Lee CY, Whitestone J, Kitzmiller WJ, Wickett RR,
Visscher MO. Quantitative model of cellulite: Threedimensional skin surface topography, biophysical characterization, and relationship to human perception. J Cosmet Sci. 2005;56:105–120.
Whipple LA, Fournier CT, Heiman AJ, Awad AA, Roth MZ, Cotofana S, Ricci JA. The Anatomical Basis of Cellulite Dimple Formation: An Ultrasound-Based Examination. Plast Reconstr Surg. 2021 Sep 1;148(3):375e-381e. doi: 10.1097/PRS.0000000000008218. PMID: 34432683.
