ANATOMY OF THE GLUTE REGION APPLIED IN PRACTICE
Content extracted from the book “Victory Against Cellulite” by Dr Roberto Chacur, Ed. AGE, 2023.
Dr. Roberto Chacur
Dr. Danuza Dias Alves
Dr. Hamilton Couto
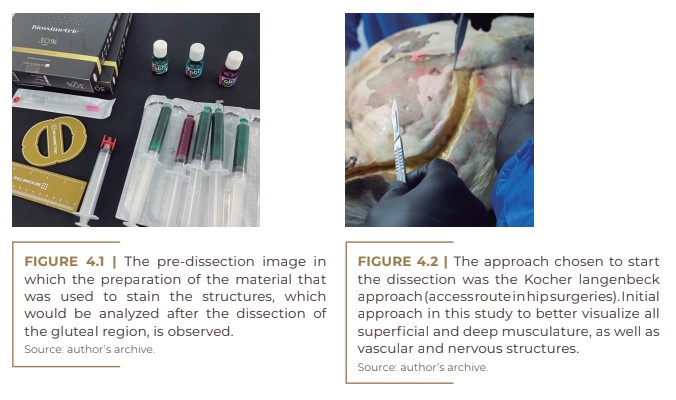
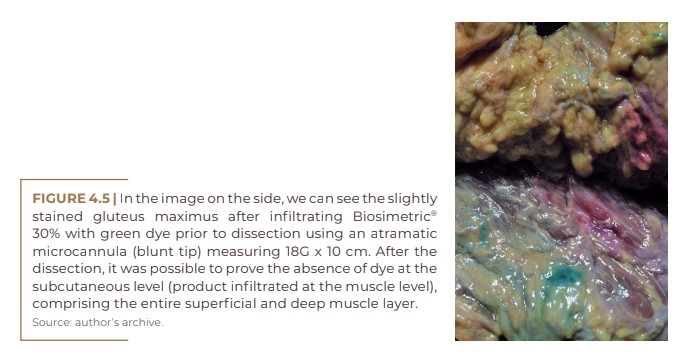
The muscle anatomy of the glutes is extremely important, especially when the patient is submitted to volumetric correction, even more so when it comes to a long-lasting product, which must be infiltrated at the intramuscular level. This plan is very important if we think about the long term, as the product needs to stay within the muscle, supporting it, and not on the skin, “weighing it down”, in addition to providing a more natural result that is imperceptible to the touch. For volumetric correction with absorbable products, in some cases, filling can and should be done subcutaneously, as well as in the treatment of cellulite, with the use of biostimulators, but always in small quantities. We shall now present the details of a dissection by the authors in fresh frozen cadavers before and after infiltration of PMMA with dye and correlating with images of anatomical drawings.
Throughout this chapter, a review of the literature will be merged with the dissection of fresh cadavers before and after application of Biosimetric® 30% with dye.
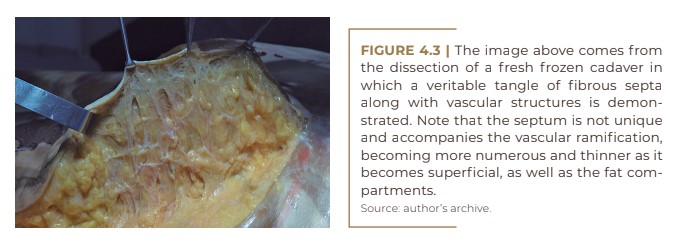
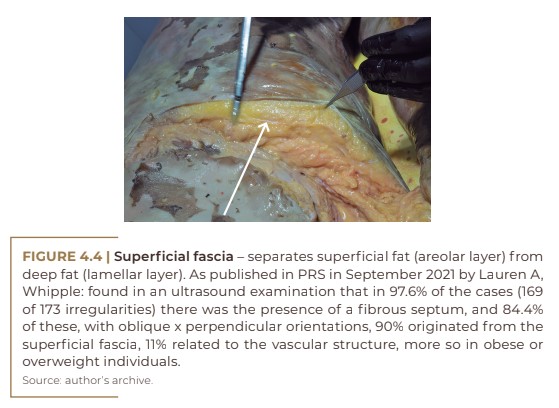
In superficial fat, we have a greater number of fat compartments with higher pressure, especially in obese or overweight patients. Consequently, cellulite irregularities appear more often, as well as greater vascular involvement, with more venous stasis and edema, which leads to an even greater increase in pressure, with more fluid retention.
See Chapters
CHAPTER 1 - DEFINITION, HISTORY AND NOMENCLATURE
CHAPTER 2 - ONLINE QUESTIONNAIRE FOR CELLULITE CLASSIFICATION
CHAPTER 3 - LIPEDEMA: DESCRIPTION, DIAGNOSIS AND TREATMENT
CHAPTER 4 - ANATOMY OF THE GLUTE REGION APPLIED IN PRACTICE
CHAPTER 6 - INJECTABLE CELLULITE TREATMENTS
CHAPTER 7 - LASER-LIPO: INVASIVE TECHNOLOGY
CHAPTER 8 - OTHER CELLULITE TREATMENTS
CHAPTER 9 - BIOSTIMULATORY EFFECTS OF MICROSPHERE INJECTIONS INTO OVERLYING SKIN STRUCTURES
CHAPTER 10 - INFLUENCE OF HORMONES ON CELLULITE: WITH EMPHASIS ON ADIPONECTIN
CHAPTER 11 - GOLDINCISION®: A MULTIFACTORIAL APPROACH TO THE TREATMENT OF CELLULITE
CHAPTER 12 - STAINS POST-GOLDINCISION®
CHAPTER 13 - ADVERSE EFFECTS AND COMPLICATIONS IN GOLDINCISION®
With the collaboration of experienced medical professionals, Dr. Roberto Chacur brings together in this book an approach around the theme ranging from the genesis of cellulite, the proper method of evaluating and classifying, associated diseases and hormonal modulation to existing treatments, what really works and why the GOLDINCISION method is considered the gold standard.
The detachment of these retractions ends up providing not only aesthetic relief, but also a reduction in local pressure, thus improving circulation and local edema, which, associated with biostimulators (which can be distributed three-dimensionally throughout the subcutaneous tissue), further promote the restructuring of collagen and implement neovascularization, which this product is known to provide.
The superficial fascia is closely related to the appearance of cellulite, which, with the gravitational force associated with skin sagging, promotes an even larger appearance.
Just below the subcutaneous tissue, we have the gluteus maximus, and its aponeurosis is in direct contact with practically all the subcutaneous tissue of the gluteus, and it is in this interval between muscle and skin that we have the irregularities.
Filling at an intramuscular level will not correct these retractions. Eventually, when performed, although projection and sagging improve, some irregularities may even become more apparent. That is, some bulges cannot be corrected at the muscular level if the reason is at the
subcutaneous level.
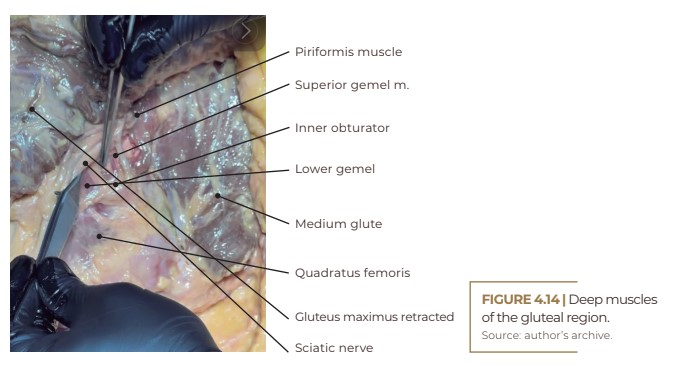
GLUTEAL REGION – MUSCULATURE, VASCULARIZATION AND INNERVATION
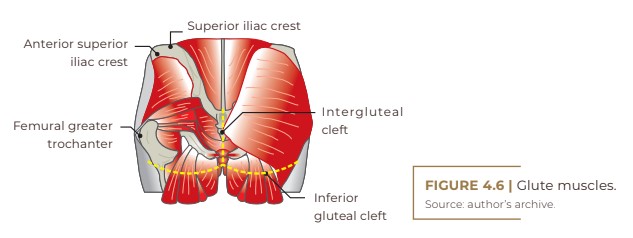
The gluteal region is the area posterior to the pelvic girdle, between the iliac crest and the inferior gluteal fold.
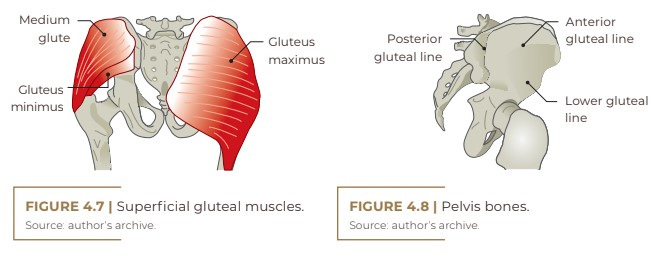
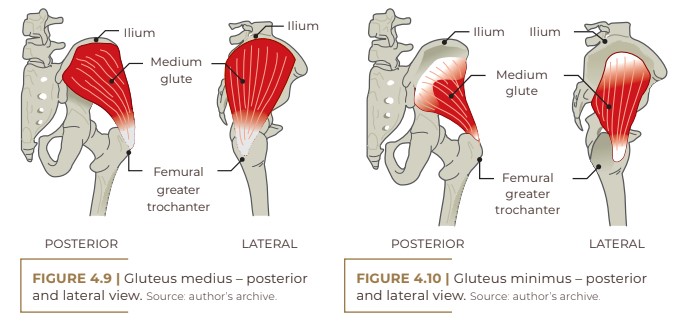
Musculature:
- Superficial gluteal muscles
- Upper glute
- Medium glute
- Lower glute
- Tensor of the fascia lata
- Deep gluteal muscles
- Piriform
- Upper and lower geminal
- Inner obturator
- Quadratus femoris
Innervation:
- Sciatic
- Upper and lower glute
- Posterior femoral cutaneous
- Pudendal
Blood vessels:
- Superior and inferior gluteal arteries (branches of the internal iliac artery)
- Superior and inferior gluteal veins (drain into the internal iliac vein)
Foramen:
- Greater and lesser sciatic pelvis (formed by the sacrospinous and sacrotuberous ligaments)
Limits:
- Superior: iliac crest
- Medial: intergluteal fold
- Lateral: an imaginary line from the anterior superior iliac spine to the greater trochanter
- Bottom: lower gluteal fold
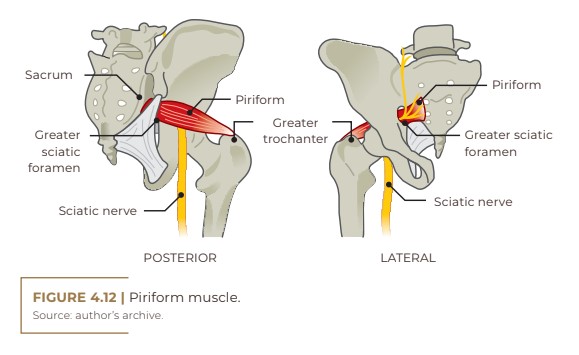
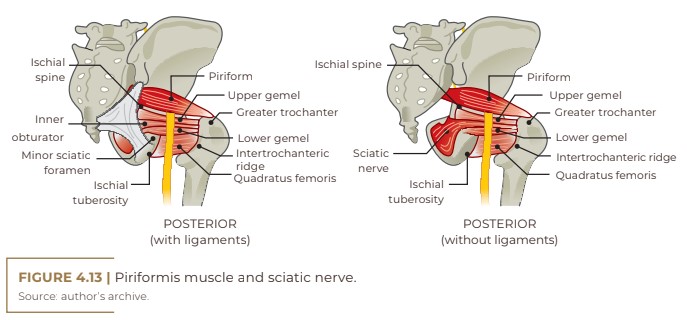
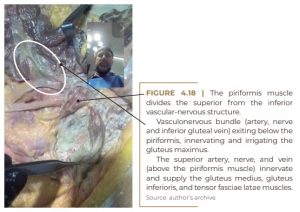
It is important to remember the anatomical relationship between the piriformis and the sciatic nerve, which is located between the piriformis and the superior gemelli. Although extremely rare, there have been reports of patients with “drooping foot”, some shortly after the procedure, probably due to anesthetic influence, and two cases with a longer evolution (60 days), one of which was associated with the
appearance of Herpes Zoster in the postoperative period, which may explain this involvement, according to reports in the literature.
Contrary to what was thought, marking the support line with the patient sitting does not exclude the possibility of reaching the sciatic nerve with the microcannula.
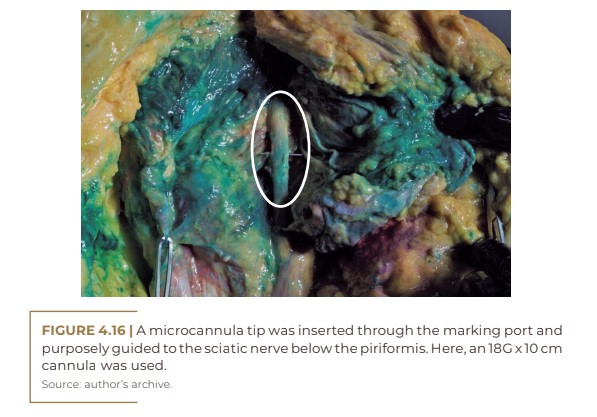
In the image above, PMMA Biosimetric® was applied at 30% with green dye, which demonstrated impregnation predominantly in the gluteus maximus and medius, and the tip of the microcannula was purposely placed there against the sciatic nerve, demonstrating that one is not getting rid of it.
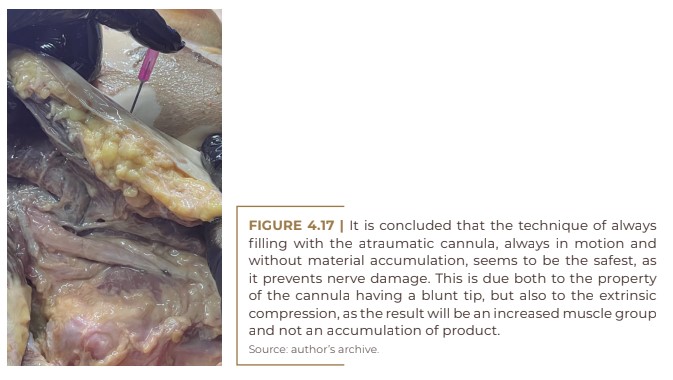
According to the literature, the depth with which the sciatic nerve is identified varies from 6.7 to 15 cm, depending on the reference point used. Therefore, we must be careful not to deepen the cannula, as there have also been reports of cases of post-procedure pudendal nerve compression syndrome, causing discomfort that affects the private parts, from the penis or clitoris to the anus, although it can radiate to the vulva or scrotum. These complications usually occur with novice physicians who inadvertently deepen the cannula in the most inferior or even medial part of the glute.
Regardless of the risk, which is small but can occur, the known cases were self-resolving, but the patient’s and family member’s anxiety can upset our work routine somewhat. Cases of “drooping foot” were observed, both under local anesthesia and, in only one case, with recovery delayed for six months.
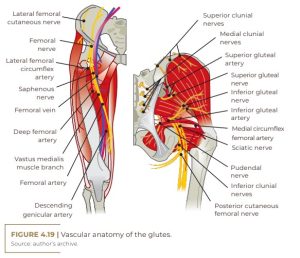
VASCULAR ANATOMY OF THE GLUTES
The two gluteal arteries (superior and inferior) arise from the internal iliac arteries and supply blood to the piriformis, quadratus femoris, and gluteus muscles. In addition, they also supply the skin of the upper thigh and gluteal regions. The medial circumflex femoral artery arises from the inferior gluteal artery.
We have no reports of ischemic or embolic vascular involvement with gluteal fillers by trained professionals using microcannulas. During the post-procedure, ecchymosis does not even develop.
In the vascular context, what we could have in the post-filling period would be an increase in vascularization, due to the properties of biostimulators, and possible visualization of telangiectasias, possibly due to the local volumetric increase and possible greater pressure in that region. As the arterial and venous drainage of the lower limbs does not pass through the gluteal region, we have no influence on the appearance of varicose veins in the lower limbs; only locally in the glutes, as venous return from the lower limbs occurs entirely.
However, in Goldincision®, we will have a vascular trauma, and this will be after the biostimulation. The trauma occurs more superficially in the subcutaneous tissue and follows the biostimulus. In this region, although there are no important structures, there will be plenty of ecchymoses and occasional hematomas.
As described in the chapter on Goldincision®, the most prevalent adverse effect is ecchymosis (100%), with occasional bruising, with the need for drainage with a needle during revision, though in some cases on the same day of the procedure, as needed. All cases are resolved with local compression, proving to be, together with the septum detachment in the most selective and profound way possible, the best preventive option for bruising and consequent stains due to residual hemosiderin. In this case, we have already tried ice, tape, among other materials, but local compression proved to be the most effective method. As such, we maintain a compressive bandage for 24 hours and modeling shorts for at least seven days.

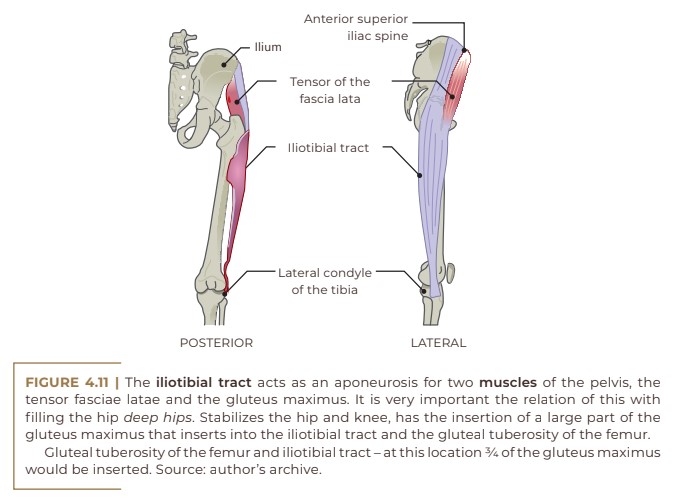
Side view – hip
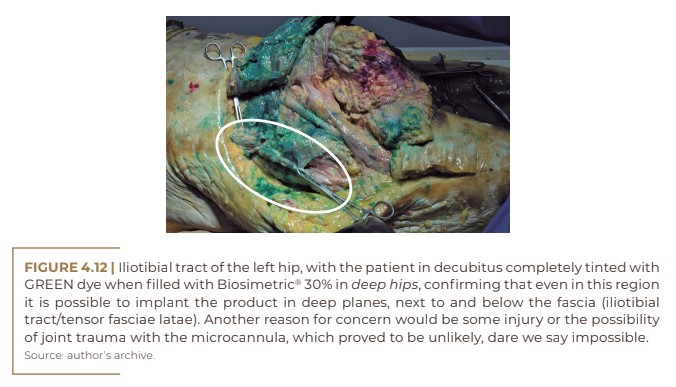
In this side view, we will see the iliotibial tract with the tensor fascia lata muscle. Very often we receive patients complaining of lateral volume in the hip or trochanteric depression and eventual transgender patients wishing to feminize the region by increasing the hip, which is not effectively achieved with other techniques. Following the precept of “supporting” and not “weighing down”, the ideal would be to infiltrate the product subfascially, as this allows for a more natural and imperceptible result, neither visually nor to the touch.
When subcutaneous in a significant amount, it is possible to immediately notice the irregularities that may appear visually already upon anesthetic infiltration. When subfascial, we have no visible irregularities, as the product is better distributed.
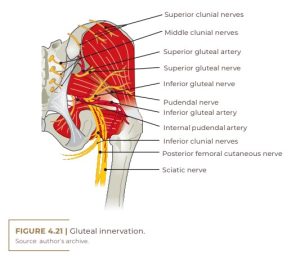
Innervation
The sensory innervation of this area is composed of the superior cutaneous nerves of the buttock or superior cluni, which arise from the lateral divisions of the dorsal branches of L1, L2 and L3. Next, in this area, we have the medium cutaneous nerves of the buttock or middle cluni, which come from the lateral divisions of the dorsal branches of S1, S2 and S3.
The lower region of the buttock is supplied by the inferior buttock nerves or inferior cluni, which arise from the posterior cutaneous nerve of the thigh. And this, in turn, originates in the ventral branches of S1, S2 and S3, which come from the sacral plexus. We also have the perianal region at the cutaneous perforating level, which also originates from the sacral plexus of the sacral branches S2 and S3, perianal region, and even the most lateral and superior region of the buttock is provided by the hypogastric nerve, which comes from the ventral branch L1. An attentive gaze at this sensory innervation shows that the superior and middle clunial nerves of the buttock do not come from the plexus, much less from the ventral branches, as a result. They are therefore branches of dorsal rami of spinal nerves. The inferior cluni originate from the sacral plexus as well as the cutaneous perforator.
Subcutaneous – treatment of irregularities
Note that the contact of the gluteus musculature with the subcutaneous tissue occurs almost entirely between the fascia of the gluteus maximus and the superolateral part with the medium; with the exception of the junction of the gluteus maximus with the gluteus medius, where there is rarely any unevenness, but occasionally it may be present. Any and all irregularities that exist are due to subcutaneous changes. To correct this, we need to act on that same level.
REFERENCES
https://www.lecturio.com/pt/concepts/regiao-glutea/. Accessed in 2022.
Hall JE, Guyton A. Tratado de fisiologia médica. 13.ed. Rio de Janeiro: Elsevier, 2017.
Moore KL. Anatomia orientada para a clínica. 7.ed. Rio de Janeiro: Guanabara Koogan, 2014.
Netter FH. Netter Atlas de Anatomia Humana. 5.ed. Rio de Janeiro: Elsevier, 2011.
Sobotta J. Atlas de Anatomia Humana. 21.ed. Rio de Janeiro: Guanabara Koogan, 2000.
